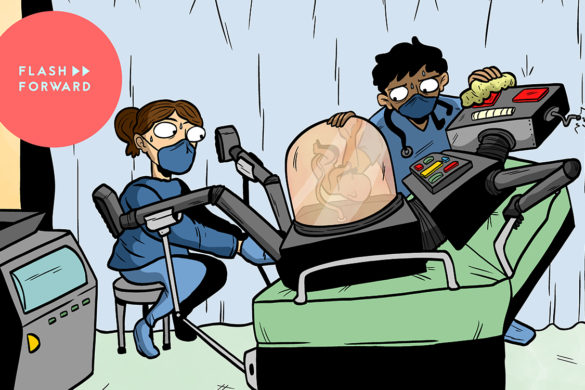
This episode we take on a future full of bioprinted replacement organs. You asked for more hopeful futures, this is about as hopeful as they get!
We start by hearing a bit about what the current organ donation market is like from Christine Gentry, who donated a kidney to a stranger. Then we talk to Dr. Anthony Atala, the Director of the Wake Forest Institute for Regenerative Medicine and of the world’s leading regenerative medicine specialists. Dr. Atala has implanted organs grown from the cells of patients themselves in clinical trials. Then Kelly and Zach Weinersmith join us to talk about what they learned while writing a chapter about bioprinting for their new book Soonish: Ten Emerging Technologies That’ll Improve and/or Ruin Everything. And finally, we get an impassioned indictment of 3D printing file formats from Meghan McCarthy, Project Lead for the NIH 3D Print Exchange.
Further reading:
- Organ Donation Statistics
- Neural and cognitive characteristics of extraordinary altruists
- Boston woman’s donation creates 3rd-longest kidney transplant chain, saving 28 people
- The Doctor and the Salamander
- How An Economist Helped Patients Find The Right Kidney Donors
- TED Talk: Printing a Human Kidney
- Rebuilding the Breast
- Soonish: Zach and Kelly Weinersmith on 10 technologies that will change everything
- Online Course Bioprinting: 3D Printing Body Parts
- Scientists 3-D Print Mouse Ovaries That Actually Make Babies
If you’re interested in becoming a living organ donor and want to know what it’s like, you can get in touch with Christine Gentry. Her email is christine.gentry at gmail.com, and she’s all about helping people understand donation.
Flash Forward is produced by me, Rose Eveleth. The intro music is by Asura and the outtro music is by Hussalonia. Our intro future voices were skillfully provided by Alyssa Mondelli, BW and Josh Kirby. The music from the intro was by Unheard Music Concepts, PC III and Soft and Furious. The episode art is by Matt Lubchansky.
If you want to suggest a future we should take on, send us a note on Twitter, Facebook or by email at info@flashforwardpod.com. We love hearing your ideas! And if you think you’ve spotted one of the little references I’ve hidden in the episode, email us there too. If you’re right, I’ll send you something cool.
And if you want to support the show, there are a few ways you can do that too! Head to www.flashforwardpod.com/support for more about how to give. But if that’s not in the cards for you, you can head to iTunes and leave us a nice review or just tell your friends about us. Those things really do help.
That’s all for this future, come back next time and we’ll travel to a new one.
▹▹▹▹▹▹▹▹▹▹▹▹▹▹▹▹▹▹▹▹▹▹▹▹▹▹▹▹▹▹▹▹▹▹▹▹▹▹▹▹▹▹▹▹▹▹▹▹▹▹▹▹▹▹▹▹▹▹▹▹▹▹▹▹▹▹
TRANSCRIPT
Rose: Hello and welcome to Flash Forward! I’m Rose and I’m your host. Flash Forward is a show about the future. Every episode we take on a specific possible… or not so possible future scenario. We always start with a little field trip to the future, to check out what’s going on, and then we teleport back to today to talk to experts about how that world we just heard might really go down. Got it? Great!
This episode, we’re starting in the year 2136.
[commercial music]
Commercial voice 1: We know you have lots of choices when it comes to your next kidney. Here are a few reasons we think that the Lensman Lab is right for you. World renowned surgeon and bio-designer Dr. Gray Lensman has successfully designed, printed and implanted over a thousand organs, from hearts to kidneys to livers. Dr. Lensman puts your comfort above everything, offering complimentary spa services, dream implantation technology for while you’re in surgery, and the highest level of aftercare. So the next time you choose an organ surgeon, choose Dr. Lensman.
[commercial music]
Commercial voice 2: Most surgeons settle for simply replacing a failed organ, but at Sharik Biosciences, we think we can do better. Dr. Lev Sharik built her practice on the principle of improvement, not just restoration. She enhances your body, so you can look and feel even better than you did before. Why settle for a replica, when you can have an improvement?
[commercial music]
Commercial voice 3: You wouldn’t let an interior decorator design your house without your input, would you? Why let doctors design your organs without any oversight? With Orgn, you can design and print exactly the organ you want from our certified repository of models, designs and upgrades. Our point and click user interface makes it easy to fully customize your new body part. Simply click, drag and print, and you’ll have an organ ready for implantation. Call now for this special offer, simply pay shipping and handling, and the printer is free! Cal 1-800-ORGN-NOW.
[[fade out]]
Rose: So, this episode we’re talking about a future in which doctors can print new organs for people cheaply and easily. This is a future that tech headlines have been predicting for ten years now. We’re always on the cusp of 3-D printing full organs, it seems. And it shows up in all kinds of science fiction too — regenerated limbs and organs are a staple of everything from Frankenstein to Elysium. And, of course, the science fiction classic Reptilicus.
Reptilicus clip: It’s a piece of skin, like leather. It’s alive! It’s loose! Reptilicus approaching the city! Repeat, Reptilicus approaching the city!
Rose: This episode we’ll talk about where we really are in the quest to print a new liver, and what stands in the way of off-the-shelf hearts.
But before we go into the future to talk about how this might impact the world, I think it’s worth understanding the state of organ donation and transplants right now. According to the U.S. Department of Health & Human Services, there are over 100,000 people in the United States currently on the waitlist for an organ, and 20 people die everyday waiting for a transplant. And while 95% of adults in the U.S. support organ donation, only 54% are signed up to be donors. And those people are signed up to donate organs after they die. Living donors are even harder to find. Often they wind up being family members or friends, and when that fails, people sometimes go to social media, asking someone… anyone to donate.
Christine Gentry: It was this random day in 2012 when I was scrolling through Facebook and an old acquaintance of mine, she posted on Facebook she said, “I’m dying. I’ve been dying of kidney failure, and all of my friends and family have tried to donate to me, and so I’m here posting on the off chance that someone I’m connected with on here feels willing to do that for me.” And I dropped everything and I messaged her. I was like, “Oh my god, Julia, I’m so sorry that we lost touch I didn’t even know you were sick. I’m absolutely willing to do that.”
Rose: This is Christine Gentry.
Christine: I am the director of teacher development and licensure for a network of public schools in Boston and all that means is that I train people who want to teach.
Rose: When Christine saw her friend Julia’s plea, she didn’t even bat an eye.
Christine: As soon as I saw Julia’s post, I was like absolutely, no hesitations. I was like OK that’s done.
Rose: There’s actually a really interesting study that came out a few years ago that suggests that the brains of kidney donors like Christine are actually different from the brains of other people.
Christine: When people don’t understand why I reacted the way that I did when I saw Julia’s post, I like to tell them not to be that impressed. This thing in my brain made it very easy. It was an absolute no brainer, pun intended.
Rose: So Christine went through all the testing and got approved to donate her kidney to Julia. But it turned out she didn’t have to.
Christine: At the very last minute Julia’s mom who had previously been rejected for a small medical reason got cleared as a donor. It was really cool, I got to watch her get her transplant.
My kidney wasn’t needed, but I got to watch it happen and see the effects of it. I mean, she wasn’t being hyperbolic in her post; she was dying. And I got to watch her get her life back. And it was really inspiring. Then a few years later she got pregnant. She had a baby, and the first picture I saw of the child, it just clicked inside of me. The only reason that this person exists, and every life that it will ever touch is because somebody was willing to donate their kidney to my friend Julia.
Rose: So she decided that even if her kidney wasn’t going to go to her friend, it should go to someone.
Christine: I just couldn’t justify not doing it for someone else.
Rose: Here is where it helps to understand how the National Kidney Registry works. For a while, kidney donations were one to one. One person needs a kidney, and another person donates one. But that requires perfect matches between those people, which can be really hard to find. Then, an economist figured out that if you could link up a bunch of pairs of people who weren’t exact matches you can figure out a swapping system.
What the National Kidney Registry does, is it uses a computer to try and find those kinds of pairs.
Christine: I could give my kidney to somebody else in the country on the condition that further down the swap chain my friend Julia would get one.
Rose: But these kinds of donation chains are still pretty complicated, and everybody has to go into surgery at the exact same time, because if one person backs out it borks the entire system. The biggest chain they could really assemble with this system was three pairs.
But after Julia got her kidney, Christine was willing to donate to anybody who was a match, she didn’t come with a person in need of a kidney attached to her. She became someone called a “non-directed donor.” These non-directed donors make it much easier to create longer chains. So when Christine entered into the computer system this second time, it found a chain for her to donate to right away.
Christine: When my surgery date was set, my chain was sixteen people long. So, I was going to give my kidney to some stranger in Ohio, and their incompatible donor would give their kidney to someone in San Diego and so forth. And so when I went into surgery, I knew that I was pulling eight people off the waitlist.
Rose: And afterwards she learned that her chain actually wound up being much larger than sixteen people.
Christine: A few months after my surgery they called me, the National Kidney Registry called me and said that the chain had kept going, and had eventually ended at fifty six surgeries. Which is incredible, right? So twenty eight people were pulled off the list because of my one decision to donate.
Rose: In fact, Christine’s kidney chain was the third longest kidney donation chain ever achieved at the time.
Have you met the person who has your kidney?
Christine: I have Skyped with her. I have not met her yet. She lives in Ohio. We didn’t get to talk that long but we stay in touch through her fiance. She’s not on social media, she’s very private. But her fiance is. Her fiance likes to tease me that I made her more stubborn. He’s like, “ever since she got that kidney from you, she’s so much more stubborn.” I’m like, “well yeah that might be me.”
Rose: I can’t wait for you to see baby photos.
Christine: Oh my God. Don’t even. You’re making me teary, I hadn’t even thought about that.
Rose: For Christine, donating a kidney was incredibly rewarding. But even though the donation chain system helps a little bit, it’s still not very efficient. And there aren’t enough people willing to donate to save everybody. Plus, those who receive donated organs have to go on immune suppressing drugs to make sure their bodies don’t reject the outsider organ.
So what if we could skip the donation part of this equation entirely? And just give people printed organs made from their own cells? Well we can. At least in some cases.
Dr. Anthony Atala: Yes in fact there are many patients already walking around with engineered organs. You know, we implanted the first organ back in 1999, so we now have a long history of implanting these.
Rose: This is Dr. Anthony Atala, the Director of the Wake Forest Institute for Regenerative Medicine. Dr. Atala implanted one of the first regenerated bladders in a patient named Luke Massala back in 2001. Here’s Luke talking about his life before the bladder implant.
Luke Massella: I was really sick. I could barely get out of bed. I was missing school. It was pretty much miserable. I couldn’t go out and play basketball at recess without feeling like I was going to pass out when I got back inside. I felt so sick. I was facing, basically, a lifetime of dialysis, and I don’t even like to think about what my life would be like if I was on that. So after the surgery, life got a lot better for me. I was able to do more things. I was able to wrestle in high school. I became the captain of the team, and that was great. I was able to be a normal kid with my friends. And because they used my own cells to build this bladder, it’s going to be with me. I’ve got it for life, so I’m all set.
Rose: That clip comes from a TED Talk that Dr. Atala did back in 2011, and after the audience saw this video of Luke on a giant screen, he came out on stage.
TED TALK:
TED Talk Host: So Luke, before last night, when’s the last time you saw Tony?
Luke: Ten years ago, when I had my surgery — and it’s really great to see him.
(Laughter)
(Applause)
Host: And Tony’s done hundreds of these?
Luke: What I know, he’s working really hard in his lab, and coming up with crazy stuff. I know I was one of the first ten people to have this surgery. When I was ten, I didn’t realize how amazing it was. I was a little kid, and I was like, “yeah, I’ll have that. I’ll have that surgery.”
Rose: Luke was one of a handful of kids who received bladders made from their own cells over 15 years ago. Which makes you think that we’re certainly well on our way to bioprinting kidneys, right? Well, not really. A structure like a bladder is relatively easy, compared to other organs.
Dr. Atala: So the way that we engineered tissues and organs has to do with how complex they are.
Rose: You can lump organs into a couple of different groups. There’s the flat stuff.
Dr. Atala: The least complex are flat structures such as skin or cartilage. Mainly because there are architecturally less complex. Mostly one major cell type.
Rose: The tubes
Dr. Atala. Blood vessels or wind pipes.
Rose: The bags
Dr. Atala: Hollow, non-tubular organs, like the bladder or the stomach. These organs architecturally are more complex. The cells are also more complex, and there’s more interaction with other organs.
Rose: And the solid hunks.
Dr. Atala: And finally, the most complex organs are the solid organs like the heart, the lung, the kidney.
So the kidneys, in fact, are one of the most complex organs. Over 20 different cell types, solid organ, multiple functions. It really is a very complex organ.
Rose: Because kidneys are so complex, there’s a lot that can go wrong with them. Which makes them, by far, organ that’s most in demand. Eighty three percent of people waiting on organ transplant lists are waiting for a kidney. Unfortunately, their complexity also makes them the hardest to bio-print.
Right now, doctors can pretty successfully print the first two groups: flat stuff and tubes. And they’re getting better at printing bags, like stomachs and bladders. But solid organs and kidneys are still elusive.
When we come back, we’ll hear a little bit about exactly why we’re still so far away from growing kidneys in the lab, and about how bioprinting might change medicine. Plus, we get really heated about file formats. And cookies.
But first, a word from our sponsors!
[[AD]]
Do you live in New York City? Do you like Flash Forward? If so, I hope you’ll join me on Saturday, November 4th for FLASH FORWARD LIVE!
Here’s the thing, I’m going to be honest with you all and say that I don’t like most live podcast tapings. Why would I sit in a room and watch people talk to each other when I can do that while in my house, in my pajamas, while eating leftovers and petting my dog? So, when I set out to make a Flash Forward live show, I wanted to make it like something you can’t get just listening to the podcast. There’s original artwork, a whole original score, an amazing actress and a story that gets weirder and weirder. Plus, the audience helps drive what happens as we travel through the future. So join me, if you can, on Saturday, November 4th for Flash Forward Live.
The show is at a really cool new event space called Caveat in the Lower East Side in Manhattan. There’s a bar and food and I’ll be giving out stickers and buttons, as well. You can get tickets at caveat.nyc, or go to flashforwardpod.com/live for more information.
Okay, I hope to see some of you in the future! Now, back to the show.
[[/AD]]
Rose: So we know that organ donation isn’t going to solve all of our organ problems. And we know that we can print some structures. But what if we could print all organs?
This is the central question of one chapter of a new book called Soonish: Ten Emerging Technologies That’ll Improve and/or Ruin Everything, written by Kelly and Zach Weinersmith.
Kelly Weinersmith: I’m Dr. Kelly Wintersmith and I’m an adjunct assistant professor at Rice University
Zach Weinersmith: And I’m Zach Weinersmith and I draw cartoons.
Kelly: Which one?
Zach: Oh yeah! Yeah. I draw a comic strip called Saturday Morning Breakfast Cereal.
Rose: Zach and Kelly’s book explores everything from asteroid mining to fusion power to programmable matter. But for now we’ll stick to the chapter on bioprinting. So we’ve talked about what we can and can’t print, but how does bioprinting work in the first place? There are actually a couple different methods, but the most common one is the 3-D printing version.
Zack: It’s something like the 3-D printer that you might have on your desktop, which is a sort of extrusion device, only instead of extruding plastic your extruding a gel that has cells suspended in it. And you sort of build something up, layer by layer, by this means. Until you have something that’s recognizable as a body part or part of a body part, like a vein, or a cornea, or someday maybe a kidney or something like that.
Kelly: And the reason this is a cool technique for making organs is because organs are made of lots of different cell types and they have capillaries and veins going through them, and they’re complicated structures. And with good 3-D printers you can be printing with multiple different things at once. So you could be putting down different kinds of cells, or different kinds of cues that those cells needed, or trying to lay out some of the vasculature. And you kind of need to do a lot of that stuff all at once as you go. Because if any cells don’t have oxygen, or nutrients, or can’t get rid of waste for a couple of hours, they’re probably going to die.
Rose: You can think of 3-D printers kind of like really fancy glue guns. You load them up with some material, and then you squeeze that material out of a nozzle. For a tabletop 3-D printer you might buy for fun, that material is usually some kind of plastic. But for organs, that material could be some goo made out of cells.
That makes it sound kind of simple. It’s… not simple at all. Just coming up with the cell-holding-goo in the fancy goo gun is incredibly hard.
Kelly: The cells need to stick together, and they need to stay together in a structure, which means you need to print them with something that’s going to hold them together. But is then later going to dissolve away as the cells create their own matrix and communicate with one another. And as you’re trying to put these cells together they need various cues. Sometimes you need to heat them, or they need to have cues so that they know where to go, or what to do, and they need to be talking to each other.
Rose: And even if you get the right cells in the printer, you have to make sure that the very act of printing doesn’t mess them up.
Kelly: You need to make sure that as it’s going through the bio-printer you’re not compressing the cells too much so that they squeeze and pop before they come out of the little tube.
Rose: Sometimes, to solve all these problems, scientists wind up adding stuff to the 3-D printing goo that you don’t really want in your final product.
Zach: The stuff that makes it easy to 3-D print something is not necessarily stuff you want in your body.
Rose: One way to imagine this is to think about cookies. Delicious 3-D printed organ cookies. Just kidding, regular cookies. Actually, we’re just talking about regular cookies.
Zach: We read the story about this guy who wanted to 3-D print shortbread, so he could bake letters and shapes and so forth. And the problem is with something like shortbread, it seems like a pretty good substance to extrude out into a 3-D printer because it’s fairly solid, but it’s not homogenous. So if you have it sitting in your little device for a while it’s going to separate. There will be chunky bits here, and smooth bits here. And so when you’re trying to extrude it smoothly, it’s not going to work well.
So what do you do, you add other substances. You add something some emulsifier to smooth it out, or maybe some other thing to thicken it up. You’re also going to remove anything that’s interesting, like chocolate chips or something, because that’s going to mess with your apparatus. Anyway, so you can keep adding these different things to your shortbread mix. And what’ll happen, and this is what happened to the guy in this story we found, is you get this really nice extruded shortbread looking stuff that just tastes awful.
Rose: The same thing goes for 3-D printed organs. To make the printing process work, scientists often add chemicals that they don’t actually want in the final product. Which means they then have to figure out a way to get those chemicals out later on.
This is just one of many hurdles that 3-D printing organs faces. Researchers still have to figure out how to get blood vessels to survive deep inside bigger chunks of tissue so that oxygen and nutrients can move in and out. As Kelly and Zach put it in their book, “it’s sort of like trying to create a factory all at once, instead of building the structure, then bringing in the machines, then hiring the employees.”
But one thing that really surprised me to learn while reading Soonish, is that one of the hurdles facing bioprinting is… file formats.
Kelly: In almost every case, when we were researching this book, what we thought we were going to learn about the technology is not what ended up being the surprising and interesting thing about the technology. So, we had expected that the problems with bio-printing were going to be the kinds of things we just talked about. And then we were talking to Dr. Jordan Miller at Rice University, and we asked, “hey are there any other problems?” And he said, “well actually, the software that’s associated with 3-D printers was made in the 80s” And so there are the these STL files that are meant for telling you about the external structure of a 3-D object. But it doesn’t specify any of the stuff that’s happening inside. And you’d like there to be interesting stuff going on inside of your liver. So that’s important. And that blew our mind, because we did not think that was going to be a limiting factor in this.
Meghan McCarthy: So I’ll say this, essentially it’s sort of my rant on STL, and how it’s lame, and how the whole 3-D printing community needs to sort of get on board with newer file formats. Which is which is a very strange passion to have.
Rose: This is Meghan McCarthy.
Meghan: I am with the office of Cyber Infrastructure and Computational Biology at the National Institute of Allergy and Infectious Diseases; part of the National Institutes of Health.
Rose: Meghan is also a project lead for something called the NIH 3D Print Exchange, which is an online repository of 3-D printing models. The project is not for bioprinting; the files they have are for printing in plastic, or some other non-biological material. But Meghan spends a lot of her time thinking about 3-D printing file formats.
Meghan: I’ll talk your ear off on that. It’s sort of my pet project right now. So you could give a 3-D file to five different people. Each person that went to print it, even on the same printer, would end up using different parameters; whether it was solid, or it was hollow, or it was a different resolution. So they might have thicker or thinner layers in the plastic or resin or whatever we’re using. When you’re able to contain those printer parameters within the file itself and ideally import them into the printer software that you’re using, i means that the print is going to be true to what the original designer intended.
Rose: So if one team designs the organ, and another team prints it, they might wind up with a heart that has thicker or thinner walls than the designer wanted. Which is obviously not a mistake you want to make with a replacement heart. The solution for most teams working on bioprinting right now, is to simply design all your their stuff.
Dr. Atala: Well, you know we have devised all our software program here because we build our own printer. So our printers are specifically designed for printing tissues and organs. Being that we designed these printers and we built them, we also had to build a software program to support them.
Rose: Other people are using coding languages that weren’t designed for 3-D printing at all.
Meghan: I know people that are that are using bio printers that actually are using Python code, which is a programming language. So instead of just adding G-code and instruction to the printer, you’re giving some giving it something much more sophisticated in a different language.
Rose: But if bioprinting is really going to be a huge movement, it’s probably not great to have each hospital using their own bespoke and proprietary software and printers.
Meghan: The bioprinting world; I think ultimately it could maybe end up with its own file format. Who knows?
Rose: Nobody I talked to thinks that bioprinted organs for the masses is coming all that soon. It’s still really hard to print even small structures, and get them to survive. There’s a startup called TeVido that prints replacement nipples for people; mainly folks who’ve had mastectomies. And it turns out it’s pretty hard to get the nubby bit of the nipple to connect to the areola skin bit. In other words, we’re not close to printing kidneys.
But one of the nice things about this future, compared to most of the other futures that we talk about on this show, is that it’s hard to think of very many specific downsides to being able to print organs for people.
Kelly: Bioprinting has not a ton of ethical concerns associated with it, or at least not a ton of ethical concerns above and beyond a typical biotech ethical concerns.
Rose: Of course, access to this kind of technology will be distributed unequally, just like all of healthcare is right now. Not everybody will be able to afford to get a regenerated organ. So maybe donated organs will continue to serve those who can’t afford a custom ones printed from their own cells.
Some people also wonder if having easily replaceable organs might change the way people treat their bodies.
Zach: In a world where you can just print off new body parts, I think if we’re alive to see it, we’re we’re going to be this people who are a little uncomfortable about the way young people might treat their bodies. If all the parts are replaceable. There might be this weird sort of social change around the idea that body parts are kind of generally disposable.
Rose: Dr. Atala doesn’t worry about that, at least not for now.
Dr. Atala: No. I mean, these technologies so complex. And of course nobody would want to go through that surgery. And of course there could be complications with the surgeries, they’re not easy, the recoveries could be tough. Patients could die receiving a vital organ, if it doesn’t work well. It’s not something that people are going to be signing up to do any time soon, unless they really need one.
Rose: And Christine, the woman who donated her kidney, laughs it off too. If receiving a kidney is anything like donating one, it’s not a procedure that you would do for fun.
Christine: So they flip you over on your side, I think. I was obviously out for this part, thank God. And they fill your entire abdomen with gas, to make room for them to see things better. And then they do these three small incisions, for the camera and the snipper guys. And then they go in there, snip all the connective tissue around the kidney, all the veins and stuff like that. And then they do kind of a four inch incision at the bottom of your abdomen. And somebody actually sticks their hand inside of you and pulls the kidney out. It’s like that scene from Indiana Jones Temple of Doom.
Rose: If we could print organs, nobody would have to go through that. In fact, nobody would donate organs anymore at all. Sometimes, I like to think about distant future archaeologists. And in this case, I imagine them coming across the bodies of humans from about, say, 1990 to 2060, and noticing that some of them are buried after having all their organs removed. And trying to figure out why that is. And why it stopped.
But you can take this future one step further, too. What if you could replace organs with better organs. There are body hackers now who are really interested in improving humans, not just replacing things. Dr. Atala is a doctor, and like most of the people currently working in bioprinting, his focus is replacing organs.
Dr. Atala: Evolution has done a pretty darn good job about being able to get us to where we are today. Right now we have literally millions, and millions, and millions of years of evolution to get these organs and tissues to work the way they do. And if you really think about it, when you sit back and realize how many things can actually go wrong with a human body any day, and they really just don’t. For the most part, you walk around with a pretty darn good set of organs. And so our goal is to basically replicate what nature has already done.
Rose: But evolution isn’t an efficient process, nor is it one that is driving towards any specific supreme being. If you were going to design a human from the ground up today, you probably wouldn’t do it the way that evolution has. You wouldn’t include the gallbladder, or make the ulnar nerve run so close to the elbow. And, have you seen human knees? You would get an F on that design project.
Kelly: Our organs came about through natural selection, the process of evolution. So they’re not necessarily the nicest solution to the problem. They’re the solution to the problem that nature ended up on. If you have really clever engineers, maybe you could make it part heart cell, part pump, and that would be even more effective and less likely to fail and more efficient. There’s no reason that your heart shape is necessarily the absolute best way to pump blood around your body.
Rose: I, personally, have a tiny bladder, and I would love a slightly bigger one, one that didn’t force me to leave the theater in the middle of every movie to pee. Usually at the most exciting part, as well. So I would definitely sign up to get my bladder replaced. And I bet that this kind of thing wouldn’t start with full organs. People already get plastic surgery to change their bodies. I have several tattoos. It’s not that far away to, say, changing big parts of your skin.
Rose: And the other thing I was thinking of, is that if you can just print new skin, then you can get a really regrettable tattoo, and it’s not that big of a deal.
Kelly: Oooh, I hadn’t thought about that. So when you graft new skin on, does it seamlessly……wouldn’t you still have a weird line…..? So I’m looking at my arm, which is covered in freckles. So if I put a new, clean, piece on there, it would look obvious. So you couldn’t completely erase your old sin, could you? But you could cover it.
Zach: You could get a whole new arm though.
Rose: Or, instead of getting tattoos, you could get cool enhanced skin replacements full of sensors, or scales, or something. This all got me thinking about how we might treat our discarded organs in the future.
So I got my IUD replaced recently, and I asked of the woman, I was like, “I would like to keep it.” The old one, because it’s kind of cool. It was inside my body, and now it’s outside my body. I haven’t had a baby, so it’s the only other time I really get to experience that.
I feel like if you were to get replacements, would people have a little collection, in their office, have their little jars of their organs, which I would want. It would be so cool.
Zach: That totally fits into my “we’re going to be weird to our grandkids” thing. It’s going to be like, “grandma keeps all her old livers, isn’t that weird?”
Rose: I am really looking forward to being the weird old grandma with a shelf full of livers that she shows to her grandkids to creep them out.
MUSIC UP
That’s all for this episode! For more information about anything we talked about on this episode you can look at the show notes, or go to flashforwardpod.com to find links. If you’re interested in becoming a living organ donor and want to know what it’s like, you can get in touch with Christine Gentry. Her email is Christine.Gentry@gmail.com, and she’s all about helping people understand donation.
Kelly and Zach Weinersmith’s book Soonish is out now, and you can totally go buy it! I truly enjoyed it, and don’t skip the introduction about why it’s hard to predict the future. This is not an ad, they didn’t pay me to say this, it’s just really good.
Flash Forward is produced by me, Rose Eveleth. The intro music is by Asura and the outtro music is by Hussalonia. Our intro future voices were skillfully provided by Alyssa Mondelli, BW and Josh Kirby. The music from the intro was by Unheard Music Concepts, PC III and Soft and Furious. The episode art is by Matt Lubchansky.
If you want to suggest a future we should take on, send us a note on Twitter, Facebook or by email at info@flashforwardpod.com. We love hearing your ideas! And if you think you’ve spotted one of the little references I’ve hidden in the episode, email us there too. If you’re right, I’ll send you something cool.
And if you want to support the show, there are a few ways you can do that as well! Head to www.flashforwardpod.com/support for more about how to give. If you give on Patreon, there are some new reward levels. I just sent out some sneak peak images about what the future swag for Flash Forward is going to look like. So you can get that if you are a five dollar donor. But if that’s not in the cards for you, you can head to iTunes and leave us a nice review or just tell your friends about us. That really does help.
That’s all for this future, come back next time and we’ll travel to a new one.






3 comments
You might want to look at the work of https://be.mit.edu/directory/linda-g-griffith
In her work, the orgrans on a chip are used for things like drug testing and research. This is cool because using human tissue for this is a lot more accurate than using animals.
[…] end of organ donation waiting lists (Listen 33:00) – This podcast explores the idea of printing (yep, PRINTING) organs from our own cells. We could completely eliminate the need for waiting lists […]
[…] Easy Bake Organs […]